BUBBLE HELMET
VENTILATOR
VIDEO DEMONSTRATION
PROBLEM

India has an estimated 40,000 working ventilators, a number experts
said will be inadequate in case there is a surge in Covid-19
infections that, in approximately 5% of the cases, sends patients to
intensive care units (ICU) with acute breathing problems.The
coronavirus attacks people's lungs, in some cases compromising their
ability to breathe as they develop pneumonia. Ventilators, which
deliver air to the lungs through a tube placed in the windpipe, are
crucial to keep these patients alive. Mechanical ventilators are
creating more problems than it is solving for ARDS patients.
What are the primary risks of a BVM/Mechanical ventilator?
Being viewed as a viable alternative to available professional care or
delaying seeking professional care. This should be viewed as an
educational resource or a last resort option only unless it’s medical
viability is proven otherwise. Community driven engineering
efforts like this run the risk of making it "too easy to be harmful"
which would be a bad outcome. Using non-invasive interfaces (such as
masks and mouth pieces) can create aerosolized viruses infecting the
medical personnel working in close proximity to the patient. This can
lead to exponential transmission of the virus. Usage should be
restricted to places where aerosolized viruses are already abundant
(lots of unmasked symptomatic individuals), COVID wards, or in
isolation.
SOLUTION

In the event that COVID-19 hospitalizations exhaust
the availability of FDA/ICMR approved ventilators. This
project documents the process of converting the available
compressed air and oxygen tanks at hospitals into a rudimentary
non-invasive pressure support ventilator that could help with
breathing during respiratory distress. It's an evolving project,
but in its current form, it most aligned with the definition of a
non-invasive pressure support BiPAP ventilator.
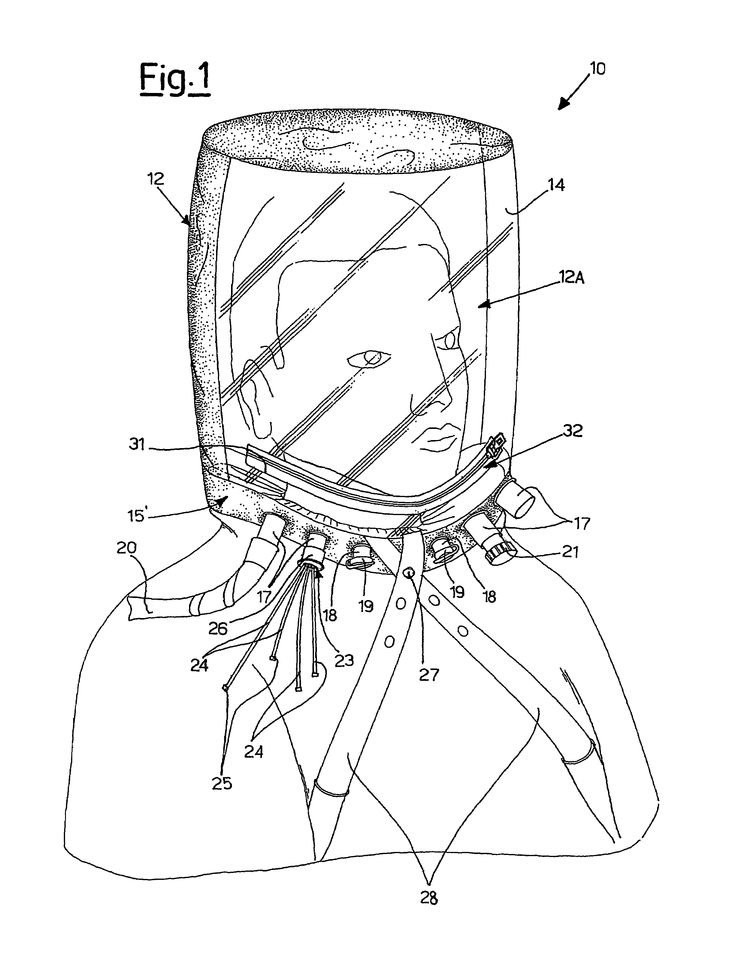
Bubble Helmets are used for patients suffering from
Acute Respiratory Distress Syndrome (ARDS) which
is also caused by COVID-19, the disease caused by the 2019 novel
coronavirus. The helmet surrounds the patient’s entire head to
supply oxygen and is sealed with a soft, airtight collar that
wraps around the neck.

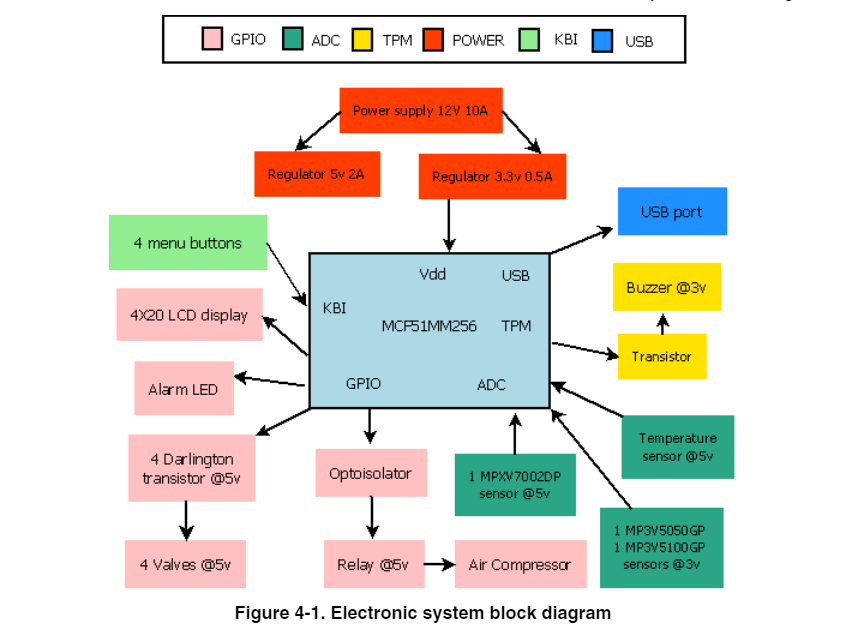
TECH STACK
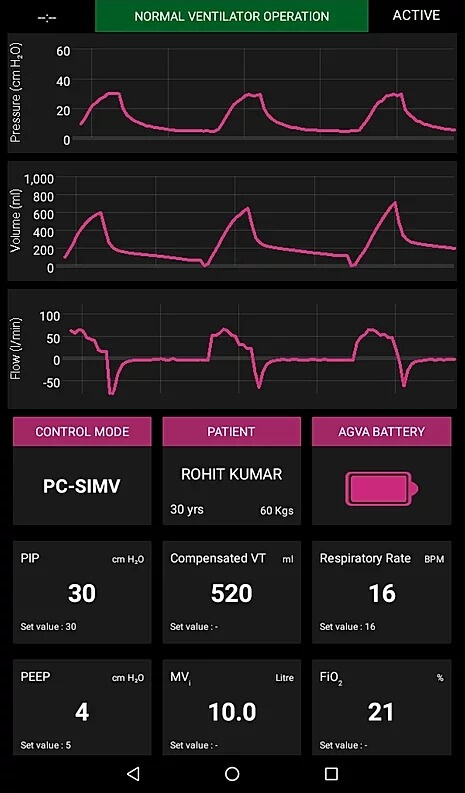
Ventilator
Air gas inlet
O2 gas inlet
Air reflux valve
O2
reflux valve
O2 metering valve
Air metering valve
Mixing
Tank
Mixed gas metering valve
Safety valve
Expiratory
flow sensor
Barometric Pressure sensor
Calibration valve
for inspiratory
pressure sensor
Inspiratory pressure
sensor
Calibration valve for expiratory
pressure
sensor
Expiratory pressure sensor
O2 sensor
Air
pressure regulator
O2 pressure regulator
CO2 sensor
Neonatal
flow Sensor
Nebulizer Mixer Valve
Nebulizer changeover
valve
Nebulizer Outlet
Bubble Helmet
Bubble Helmet components can be made efficiently with 3D printing
and industrial grade tools.
Medical Grade Plastic
Material (Anyone can be used depending on the supply) :
Sustanat
PC MG (Polycarbonate)
FibreTuff PAPC: The 3D printing
material will be used to make Class A, Class B and Class C medical
devices.
Medical grade Non-Latex Synthetic
RubberNeopreneBuna-N

PROTOTYPING
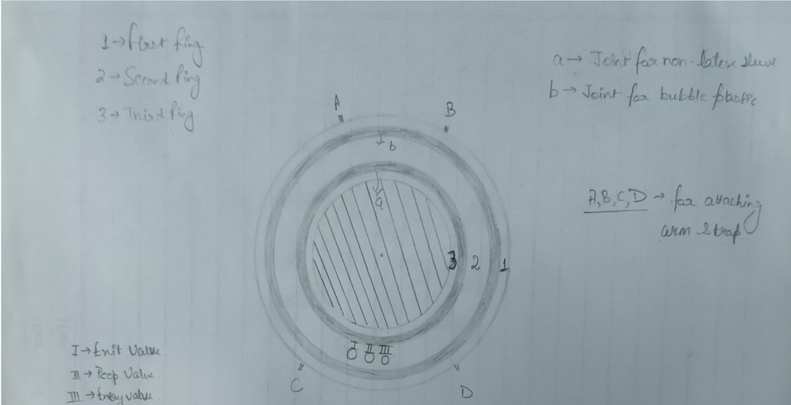
Initial design
Wireframe Desgin
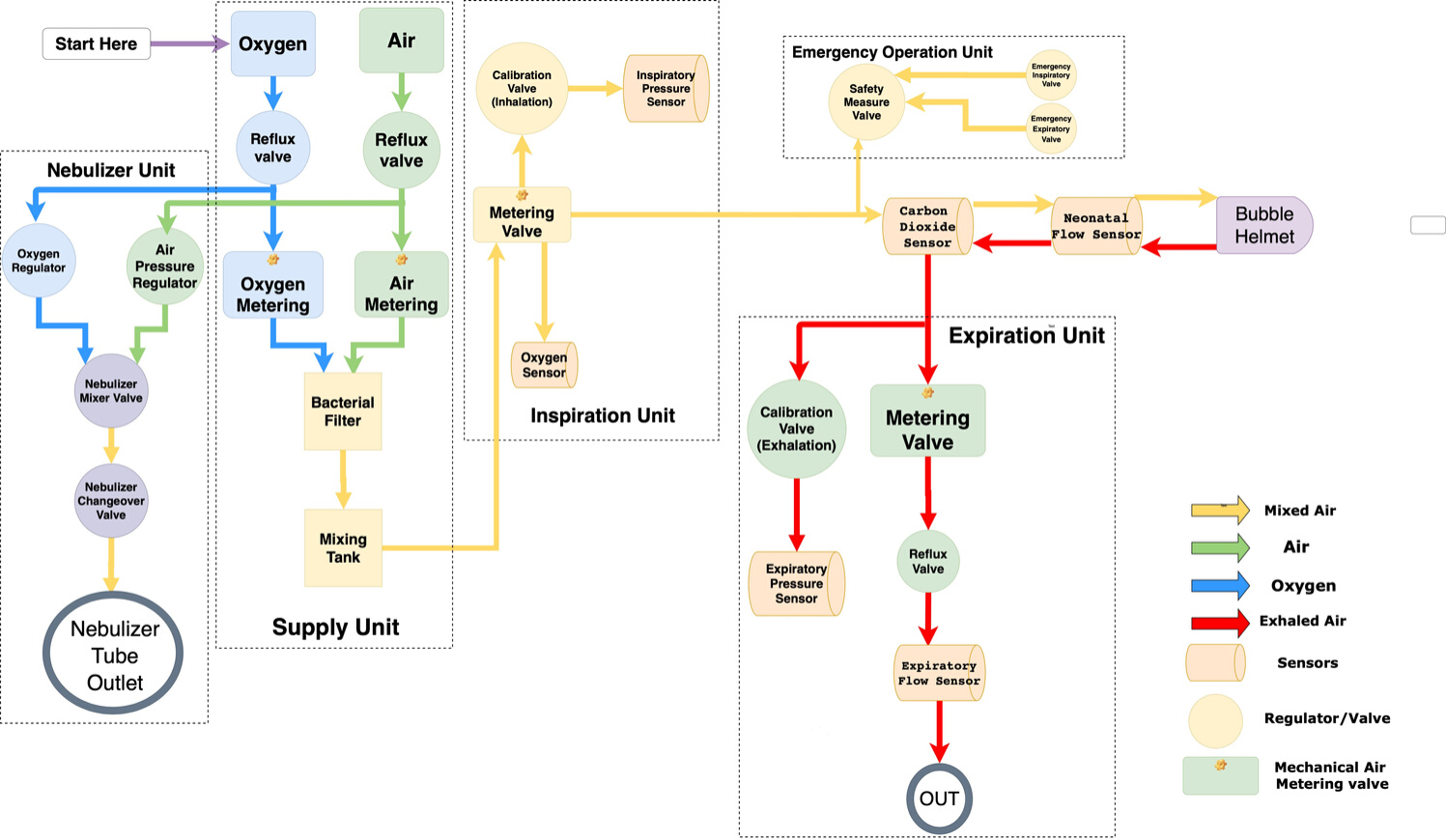
Pneumatic schematic of the Ventilator.
1. Gas-mixture
and gas-metering assembly. Gas from the supply lines enters the
ventilator via the gasinlet connections for oxygen and air . Two
nonreturn valves prevent one gas from returning to the supply line of
the other gas. Mixing takes place in the tank and is controlled by two
valves. Inspiratory flow is controlled by a third valve.
2.
Respiratory unit consists of safety valve and two nonreturn valves .
In normal operation, the safety valve is closed so that inspiratory
flow is supplied to the patient’s lungs. During standby, the safety
valve is open and enables spontaneous inspiration by the emergency
breathing valve. The emergency expiratory valve provides a second
channel for expiration when the expiratory valve is blocked.
3.
Expiratory unit consists of the expiratory valve and a nonreturn
valve. The expiratory valve is a proportional valve and is used to
adjust the pressure in the patient circuit. In conjunction with the
spring-loaded valve of the emergency air outlet, the nonreturn valve
prevents pendulum breathing during spontaneous breathing.
4.
Expiratory flow sensor.
5. Barometric pressure sensor.
Conversion of mass flow to volume, body temperature and pressure
saturated (BTPS) requires knowledge of ambient pressure.
6.
Pressure measurement assembly. Pressure in the patient circuit is
measured with two independent pressure sensors .
7.
Calibration assembly. The pressure sensors are regularly zero
calibrated by connection to ambient pressure via the two calibration
valves.
8. Oxygen sensor.
9. Medication
nebulizer assembly
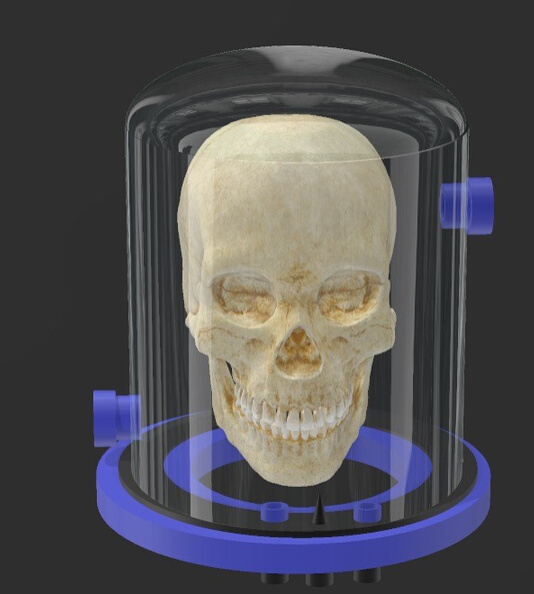
Schematics of the helmet
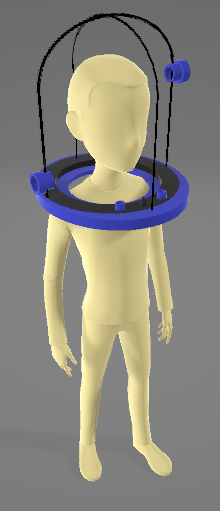
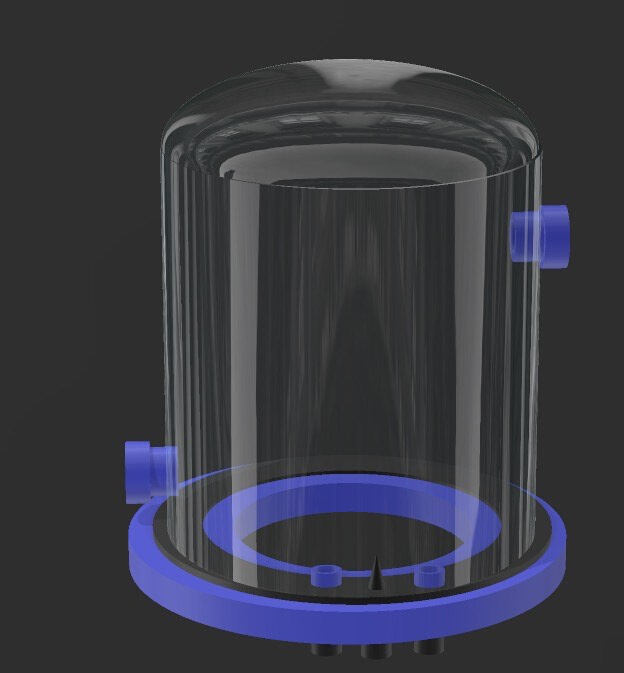
The primary function of the Bubble Helmet is to provide the
patient with oxygen rich air (as per the patient's requirement) and
also at a higher atmospheric pressure (If required).
The
Helmet is provided with Entry and Exit valves to facilitate the flow
of air inside the Bubble Helmet.
Also two emergency holes
are given in the plastic bubble acting as emergency valves to supply
air to the patient using an ambu bag.

HARDWARE
CAPABILITIES
Ventilator
This design can have a
programmable breathing rate (ex: 10-30
cycles/min.)
It can have a programmed
Positive End-Expiratory Pressure (PEEP).
The Ventilator is physically able to hit
a peak air pressure of up to 45 cm of H2O.
PIP (Positive Inspiratory Pressure) :
This gives the range of pressure we can have in the
hyperbaric chamber (Bubble).
(Range: 12 to 30 cm of H20)
Medication
nebulizer assembly-It is easy and
pleasant to breathe the medicine into your lungs this
way. It is lacking in many other ways, but it is possible that this
limited functionality could be helpful when better care is not
available. It is also a starting point for making progress. Critical
features can be added over time.
Bubble Helmet
The primary function of the Bubble Helmet is to provide the patient
with oxygen rich air (as per the patient's
requirement) and also at a higher atmospheric pressure (If
required).
The Helmet is provided with
Entry and Exit valves
to facilitate the flow of air inside the Bubble Helmet.
Also
two emergency holes
are given in the plastic bubble acting as emergency valves to supply
air to the patient using an ambu bag.
The
patient does not feel claustrophobic, which is a common drawback of
face mask based ventilators.
WHY WE?
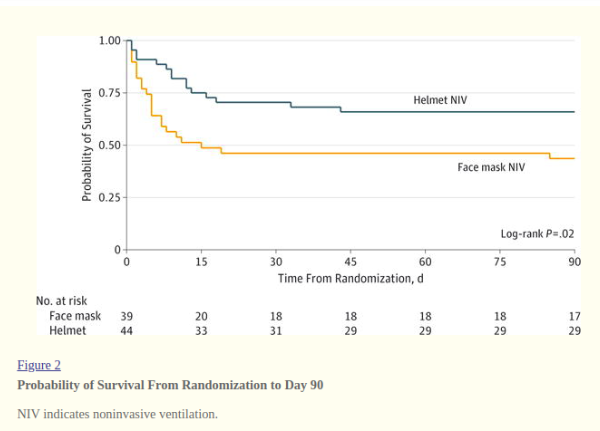
Noninvasive ventilation (NIV) with a face mask is
relatively ineffective at preventing endotracheal intubation in
patients with
acute respiratory distress syndrome (ARDS). Delivery of NIV with a helmet may be a superior strategy for
these patients.Delivering NIV via a helmet interface–a transparent
hood that covers the entire head of the patient with a soft
collar
neck seal, confers several advantages over face mask
including improved tolerability and less air leak due to the
helmet’s lack of contact with the face. Therefore, the helmet’s
design
may allow
increased titration of positive airway pressures
without substantial air leak. This could reduce intubation rates
and extend the benefits of NIV to more patients with ARDS.
The
patient in turn feels less claustrophobic, spends less time at the
ICU and can sooner get rid of the ventilator than the traditional
mask.
Ventilator Powered Bubble Helmet is a much needed rescue from the
traditional masks and ventilators in the time of a crisis.
Its
ability to most of all create a nonclaustrophobic
environment for the patient, who is already under life support is
one of the greatest advancements in medical masks. Along with that
the cost effectiveness and advantage to the patients and doctors
citing its unique shape and design is a winwin deal. COVID-19
crisis is amongstthe worst crisis ever faced by the modern world.
Moreover the consequences of the pandemic will be far more
destructive than the current crisis. It is essential to savethe
resources available for any future need. The product tick these
boxes and since are 3-D printed they are sustainable, and cheap.
This product thereby, stands toe-toe in facing the challenges
posed by this pandemic